Designing a Decision-Making Model for Emergency Evacuation of Hospitals in Crisis Conditions
Keywords:
Hospital evacuation, crisis decision-making, emergency preparedness, structural equation modeling, disaster management, healthcare resilienceAbstract
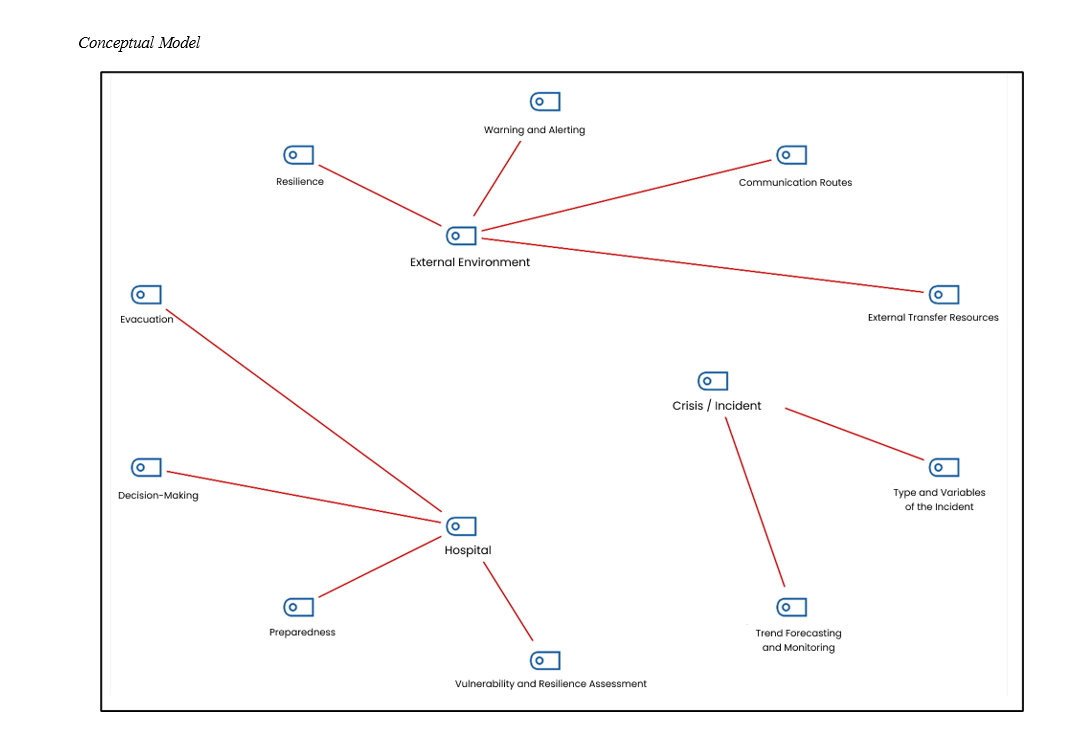
This study aimed to design a comprehensive and empirically validated decision-making model for the emergency evacuation of hospitals in crisis conditions, integrating environmental, institutional, and threat-related variables. This applied research employed a mixed-methods design. In the qualitative phase, data were gathered through semi-structured interviews with seven crisis and hospital management experts, combined with thematic analysis using Braun and Clarke’s six-step method and supported by MAXQDA software. These interviews, along with an extensive literature review, were used to identify themes and build the initial conceptual model. The quantitative phase involved the development and distribution of a validated researcher-made questionnaire, which was administered to 440 healthcare managers, decision-makers, and crisis specialists. Factor analysis, Cronbach’s alpha, and structural equation modeling (SEM) using LISREL were employed to assess the model’s validity, reliability, and predictive power. The findings confirmed the significance of three primary dimensions—external environment, hospital-related factors, and threats/crises—in shaping emergency evacuation decisions. The coefficient of determination (R²) for the external environment and hospital factors was 0.90 each, indicating very high explanatory power, while threats and crises showed a moderate R² of 0.45. All 59 questionnaire items had strong factor loadings, and Cronbach’s alpha values for each construct exceeded 0.94, confirming the tool’s reliability. Path analysis demonstrated statistically significant direct effects: external environment (β = 0.59, t = 26.47), hospital factors (β = 0.55, t = 31.03), and threat/crisis conditions (β = 0.45, t = 15.90). The study presents a validated, multidimensional model for hospital evacuation decision-making that reflects both theoretical soundness and practical applicability. The model offers a structured approach for healthcare systems to improve emergency preparedness and response capacity by aligning institutional readiness with external and situational demands.
References
Afulani, P. A., Gyamerah, A. O., Nutor, J. J., Laar, A., Aborigo, R. A., Malechi, H., Sterling, M., & Awoonor-Williams, J. K. (2021). Inadequate preparedness for response to COVID-19 is associated with stress and burnout among healthcare workers in Ghana. PLoS One, 16(4), e0250294. https://doi.org/10.1371/journal.pone.0250294
Ahmady, S., Shahbazi, S., & Heidari, M. (2020). Transition to Virtual Learning During the Coronavirus Disease–2019 Crisis in Iran: Opportunity or Challenge? Disaster Medicine and Public Health Preparedness, 14(3), e11-e12. https://doi.org/10.1017/dmp.2020.142
Amjadi, S., & Rahmani, Z. (2014). Hospital Disaster Planning Guide. International Journal of Current Life Sciences, 4(5).
Argyriadis, A., Ioannidou, L., Dimitrakopoulos, I., Gourni, M., Ntimeri, G., Vlachou, C., & Argyriadi, A. (2023). Experimental Mindfulness Intervention in an Emergency Department for Stress Management and Development of Positive Working Environment. Healthcare, 11(6), 879. https://doi.org/10.3390/healthcare11060879
Boin, A., & McConnell, A. (2007). Preparing for Critical Infrastructure Breakdowns: The Limits of Crisis Management and the Need for Resilience. Journal of Contingencies and Crisis Management, 15, 50-59. https://doi.org/10.1111/j.1468-5973.2007.00504.x
Cuthbertson, J. (2023). Ethical Decision Making in Disaster and Emergency Management: A Systematic Review of the Literature. Prehospital and Disaster Medicine. https://doi.org/10.1017/s1049023x23006325
Essien, A. E., & Petrounias, I. (2022). An Artificial Intelligence (AI)-Based Decision-Making Framework for Crisis Management. In M. Ali (Ed.), Future Role of Sustainable Innovative Technologies in Crisis Management (pp. 84-98). IGI Global. https://doi.org/10.4018/978-1-7998-9815-3.ch007
Fazeli Veisari, E., Norashrafodin, S. M., & Fazeli Veisari, M. (2021). Investigating the Mediating Role of Strategic Preparedness for Crisis Management in Islamic Azad Universities of Mazandaran Province: The Relationship between Organizational Agility and Employee Mental Health with Productivity. Modern Research in Performance Evaluation.
Fühner, J., Schmidt, S. L., & Schreyer, D. (2021). Are diversified football clubs better prepared for a crisis? First empirical evidence from the stock market. European Sport Management Quarterly, 21(3), 350-373. https://doi.org/10.1080/16184742.2020.1862273
Ghandi, M., & Roozbahani, A. (2019). Tehran's Drinking Water Supply Management in Pre Crisis Situations Using the Fuzzy PROMETHEE II Method. Journal of Water and Wastewater; Ab va Fazilab ( in persian ), 30(4), 1-15. https://doi.org/10.22093/wwj.2018.133679.2692
Hossein-Sadrabadi, I. (2023). Legal System for the "Health Emergency" Status: Management of the COVID-19 Epidemic in France. Quarterly Journal of Legal Research(2).
Jannat, F., Khorasani‐Zavareh, D., Allahbakhshi, K., Aghazadeh-Attari, J., Nateghinia, S., & Mohebbi, I. (2022). The Policy Gap and Inefficiency in Public Volunteers’ Response to Assist the Hospitals After Natural Disasters in Iran: A Grounded Theory Methodology. Disaster Medicine and Public Health Preparedness, 17. https://doi.org/10.1017/dmp.2022.53
Maksimović, G. (2024). Application of analytical hierarchy process for emergency managers selection. Journal of Decision Analytics and Intelligent Computing, 4(1), 253-262. https://doi.org/10.31181/jdaic10022122024m
Mohtady Ali, H., Ranse, J., Roiko, A., & Desha, C. (2023). Enabling transformational leadership to foster disaster‐resilient hospitals. International journal of environmental research and public health, 20(3). https://doi.org/10.3390/ijerph20032022
Nguyen, V. K., Pyke, J., Gamage, A., De Lacy, T., & Lindsay-Smith, G. (2022). Factors influencing business recovery from compound disasters: Evidence from Australian micro and small tourism businesses. Journal of Hospitality Tourism Management, 53, 1-9. https://doi.org/10.1016/j.jhtm.2022.08.006
Ortíz‐Barrios, M., Gül, M., López‐Meza, P., Yücesan, M., & Navarro-Jiménez, E. (2020). Evaluation of Hospital Disaster Preparedness by a Multi-Criteria Decision Making Approach: The Case of Turkish Hospitals. International Journal of Disaster Risk Reduction, 49, 101748. https://doi.org/10.1016/j.ijdrr.2020.101748
Pudineh, M., Miri, G. R., & Anvari, M. R. (2022). Analysis of the position of crisis management organizations in increasing urban resilience (Case study: Zabol city). Emergency Management, 11(1), 129-140. https://www.joem.ir/article_251426_a354a4ff88622571c423fd906ca88af1.pdf
Rad, E. B., & Kojouri, K. K. (2021). Strategic Preparation for Crisis Management in Relation With Organizational Learning and the Mediating Role of Social Innovation and Altruism in the Red Crescent Society, Gilan, Iran. Journal of Rescue and Relief. https://doi.org/10.32592/jorar.2021.13.2.1
Siddiqi, S. M., Kareddy, V., Uscher‐Pines, L., & Chari, R. (2023). Building Public Health Emergency Preparedness, Response, and Recovery Capabilities Through Disaster Citizen Science: Perspectives From Local Health Department, Academic, and Community Representatives. Journal of Public Health Management and Practice, 29(4), 473-486. https://doi.org/10.1097/phh.0000000000001686
Un, A., Leoni, G., & Stacchezzini, R. (2023). The effect of organizational characteristics on the perceptual performance of emergency management organizations. Journal of Emergency Management, 24(3), 325-337.
Velner, T., Rubinstein, Z., & Adini, B. (2023). Organizational Resilience Among Health Organizations in Israel. Prehospital and Disaster Medicine, 38(S1), s143-s143. https://doi.org/10.1017/s1049023x23003758
Yaghoubi, T., Ardalan, A., Khorasani, D., Khankeh, H., Nejati, A., & Ebadi, A. (2017). Decision-Making on Hospital Evacuation in Disaster and Emergencies. Iran Red Crescent Med. https://doi.org/10.5812/ircmj.14214
Downloads
Published
Submitted
Revised
Accepted
Issue
Section
License
Copyright (c) 2025 Saeed Amjadi; Saeed Sayad Shirkesh, Mina Jamshidi (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.