Explaining the Model of Antecedents and Consequences of a Healthy Organization in the Ministry of Interior
Keywords:
organizational health, healthy organization, Ministry of InteriorAbstract
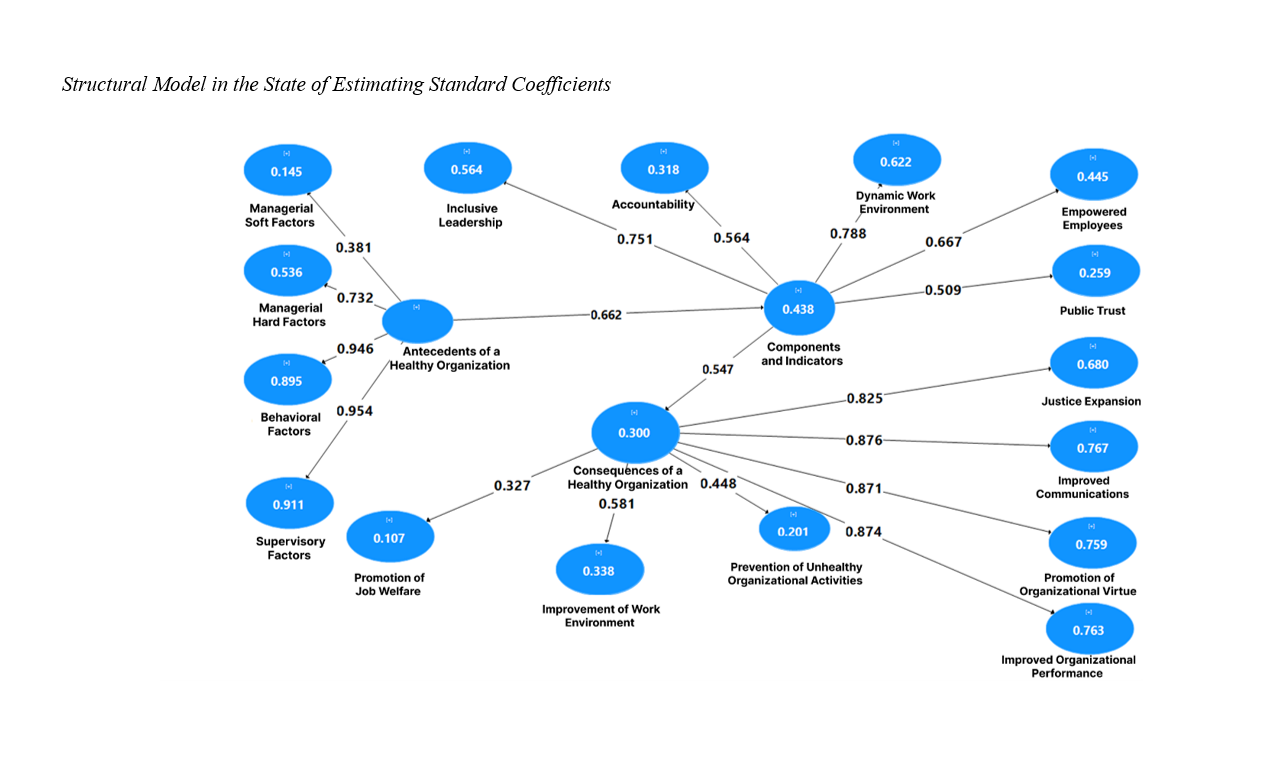
This study was conducted with the aim of explaining the model of antecedents and consequences of a healthy organization in the Ministry of Interior. From the perspective of purpose, the present research is applied, and in terms of method, it is descriptive–survey. The statistical population consisted of all deputy ministers and general directors of provincial governorates, as well as governors and district governors of East Azerbaijan, West Azerbaijan, and Ardabil provinces. The sample size was estimated at 146 individuals using Cochran’s formula, and they were selected through stratified random sampling. The data collection tool was a researcher-made questionnaire. The research variables were tested using structural equation modeling through PLS3 and SPSS software. The results showed that at a 99% confidence level, there is a positive and significant relationship between antecedents, consequences, and the components of a healthy organization, and that all indices possess strong explanatory power.
References
Alaei, F., Ahghar, G., & Fathi Vernosfaderani, L. (2024). Identification and Explanation of Organizational Health Dimensions and Components among Middle School Teachers in Tehran. iase-idje, 7(2), 36-42. https://doi.org/10.61838/kman.ijes.7.2.5
AlHamad, A., Alshurideh, M., Alomari, K., Kurdi, B., Alzoubi, H., Hamouche, S., & Al-Hawary, S. (2022). The effect of electronic human resources management on organizational health of telecommunications companies in Jordan. International Journal of Data and Network Science, 6(2), 429-438. https://doi.org/10.5267/j.ijdns.2021.12.011
Andishmand, V., & Sharifzadeh Mahani, M. (2019). Qualitative Analysis: Experienced Perceptions of Teachers on Dimensions and Components of a Healthy School. Quarterly Journal of New Research Approaches in Management and Accounting, 3(21), 14-20. https://majournal.ir/index.php/ma/article/view/271
Asghari, A., & Farahbod, F. (2021). Developing a Model for Organizational Health at Islamic Azad University, Tabriz Branch. The Second National Conference on New Researches in Management, Economics, and Accounting, Ahvaz.
Astriawati, N., Wibowo, W., Santosa, P. S., Hartanto, B., & Setiyantara, Y. (2023). Path Analysis in the Application of Occupational Health and Safety in the Ship Machinery Laboratory. Jurnal Penelitian Pendidikan Ipa, 9(11), 9713-9719. https://doi.org/10.29303/jppipa.v9i11.4666
Aust, B., Moller, J. L., Nordentoft, M., Frydendall, K. B., Bengtsen, E., Jensen, A. B., & Jaspers, S. O. (2023). How effective are organizational-level interventions in improving the psychosocial work environment, health, and retention of workers? A systematic overview of systematic reviews. Scandinavian Journal of Work, Environment & Health, 49(5), 1-14. https://doi.org/10.5271/sjweh.4097
Bleier, H., Lützerath, J., & Schaller, A. (2023). Organizational facilitators and barriers for participation in workplace health promotion in healthcare: A qualitative interview study among nurses. Frontiers in psychology, 14, 1101235. https://doi.org/10.3389/fpsyg.2023.1101235
Di Fabio, A. (2017). Positive healthy organizations: Promoting well-being, meaningfulness, and sustainability in organizations. Frontiers in psychology, 8, 1938. https://doi.org/10.3389/fpsyg.2017.01938
Farmanova, E., Bonneville, L., & Bouchard, L. (2018). Organizational health literacy: review of theories, frameworks, guides, and implementation issues. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 55. https://doi.org/10.1177/0046958018757848
Hadian, S., Yarmohammadian, M., & Shaarbafchizadeh, N. (2023). The organizational health components for small-sized health-care organizations: A systematic review. Journal of education and health promotion, 12(1), 37. https://doi.org/10.4103/jehp.jehp_1307_21
Hamouche, S. (2023). COVID-19 and employees' mental health: stressors, moderators and agenda for organizational actions. Emerald Open Research, 1(2), 1-12. https://doi.org/10.1108/EOR-02-2023-0004
Hosseini Doronkalayi, S. Z. (2023). Identifying Dimensions of Organizational Health among Employees of Coastal Cities of Mazandaran Police Command (Case Study: Cities of Sari, Babolsar, Noor, Mahmoudabad, and Nowshahr). Quarterly Journal of Mazandaran Police Science, 14(1), 53-68. https://www.joem.ir/article_718743.html?lang=fa
Jamshidian, M. A., Mirsapasi, N., & Daneshfard, K. (2020). Designing an Organizational Transparency Model Towards Administrative Health System. Quarterly Journal of Standard Management and Quality, 10(3), 1-41. https://doi.org/10.22034/jsqm.2020.254650.1258
Javanshakt, S., Mohammadi, M., & Rezaeifar, H. (2023). Designing a Managerial Competency Model Based on Organizational Health with a Mixed-Methods Approach. Journal of Transformational Management Research, 15(1), 268-300. https://doi.org/10.22067/tmj.2023.76755.1306
Kapur, R. (2023). Promotion of a Healthy Work Culture is the Key in Leading to Up-gradation of the overall Structure of the Organizations. International Journal of Information, Business and Management, 15(1), 116-125. https://search.proquest.com/openview/cb544bc81aa3f9a297010f939afb892d/1?pq-origsite=gscholar&cbl=2032142
Karamati, R., Tanhai Rashvanlu, F., Kimiaei, S. A., & Delpasand, R. (2019). Focal Analysis of the Relationship between School Organizational Health and Quality of Life of Primary School Teachers. Quarterly Journal of Rooyesh Psychology, 8(11), 133-140. http://frooyesh.ir/browse.php?a_id=1603&slc_lang=fa&sid=1&printcase=1&hbnr=1&hmb=1
Kargar, R., Ghaffari, R., & Ahmadi, M. (2020). Presenting a Model of a Healthy Organization in Combating Administrative Corruption from the Perspective of Nahj al-Balagha. Quarterly Journal of Nahj al-Balagha Studies, 19(1), 11-36. https://www.nahjmagz.ir/&url=http:/www.nahjmagz.ir/article_122556.html
Koinig, I., & Diehl, S. (2021). Healthy leadership and workplace health promotion as a pre-requisite for organizational health. International journal of environmental research and public health, 18(17), 9260. https://doi.org/10.3390/ijerph18179260
Liu, H. C., Wang, J. H., Zhang, L., & Chen, Q. Y. (2024). An integrated model for occupational health and safety risk assessment based on probabilistic linguistic information and social. https://doi.org/10.1080/01605682.2023.2242371
Ma'dani, J. (2022). Conceptual Linkage between Organizational Transparency and Healthy Organizational Culture in Governmental Institutions: A Case Study of Supervisory Organizations of the Judiciary. Quarterly Journal of Organizational Culture Management, 20(4), 801-825. https://doi.org/10.22059/jomc.2022.335126.1008385
Montazeri, M., & Ferdosipour, L. (2018). The Effect of Organizational Health on Job Performance of Employees. Quarterly Journal of Management Studies in Improvement and Transformation, 27(90), 45-64. https://doi.org/10.22054/jmsd.2019.9395
Mousavi, S. J., & Mousavi Gilani, S. R. (2023). Examining the Relationship between Organizational Health, Creativity, and Productivity of Employees at the General Directorate of Sports and Youth of Sistan and Baluchestan Province. Quarterly Journal of Organizational Behavior Management in Sports, 10(1), 29-39. https://doi.org/10.30473/fmss.2023.65048.2465
Pouyan, A., Safari, Y., & Naderi, N. (2023). Assessing the Predictability of Organizational Health by Eight Organizational Climate Dimensions: A Case Study of Kermanshah University of Medical Sciences. Quarterly Journal of Management Strategies in Health System, 8(1), 60-76. https://doi.org/10.18502/mshsj.v8i1.12890
Seyedi Taji, S. M., Khatir Pasha, K., & Fallah, V. (2023). Identifying Factors Affecting the Creation of a Healthy Organization Based on Collective Participation (Case Study: Mazandaran Industry, Mine and Trade Organization). Quarterly Journal of Supervision and Inspection, 17(8), 61-100. https://doi.org/10.22034/si.2023.101849
Shipman, K., Burrell, D. N., & Huff Mac Pherson, A. (2023). An organizational analysis of how managers must understand the mental health impact of teleworking during COVID-19 on employees. International Journal of Organizational Analysis, 31(4), 1081-1104. https://www.emerald.com/insight/content/doi/10.1108/IJOA-03-2021-2685/full/html
Torabian Badi, G., Soltani, I., & Davazdeh Emami, H. (2023). An Organizational Health Model Based on Trust in the Iranian Aviation Industry. Quarterly Journal of Social Studies in Tourism, 11(11), 209-232. https://doi.org/10.61186/journalitor.37481.11.23.209
Torkzadeh, J., Safaei, F., & Mozginejad, S. (2023). Simultaneous Modeling of Relationships between Leadership Styles, Readiness for Change, and Organizational Health: A Case Study of Shiraz University. Quarterly Journal of Educational Sciences, 30(2), 81-98. https://doi.org/10.22055/edus.2022.38658.3278
Wang, Y., & Wang, Y. (2024, November 17-19, 2023). The Impact of Transformational Leadership on Organizational Health Based on Structural Equation Modeling. In Proceedings of the 5th International Conference on Economic Management and Model Engineering, ICEMME 2023,
Xenidis, Y., & Theocharous, K. (2014). Organizational health: Definition and assessment. Procedia Engineering, 85, 562-570. https://www.sciencedirect.com/science/article/pii/S187770581401950X
Downloads
Published
Submitted
Revised
Accepted
Issue
Section
License
Copyright (c) 2025 Ghader Khodaveirdizadeh, Jafar Beikzad, Hossein Emari, Yusuf Beighzadeh (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.